Hernia Repair Options
Hernia Repairs and Treatment Options
Not all hernias require repair. Small hernias may safely be observed in certain situations. All hernias will get bigger over time but the rate at which they enlarge is variable. Which hernias require surgery is an individual decision between the patient and surgeon.
Diagnostic Tests
The following tests may be used to give your physician a clear understanding of your hernia. (Some blood tests and/or an echocardiogram – or EKG - may be required before you have anesthesia for a surgery.)
- Computerized tomography (CT) scan: This diagnostic X-ray test utilizes computer software to create a detailed,three-dimensional picture of your abdomen. A CT scan is commonly used to detect abnormalities or disease inside the abdomen. It is sometimes used to find a hernia that is not obvious during the physical exam.
- Ultrasound: Sound waves are used to make images of organs and structures inside the body, without the use of X-rays. An ultrasound may be used to find a hernia that is not obvious during the physical exam.
Nonsurgical Treatments
For mild hernias, and other diagnoses including rectus diastasis and athletic pubalgia (sports hernia), your physician may prescribe physical therapy, with a focus on core strengthening exercises with special attention given to deep abdominal muscles, like the transversus abdominis. Supportive garments or abdominal binders may also be advised, especially for postpartum recovery.
For a sports hernia diagnosis, rest and activity may be prescribed, as well as anti-inflammatory medications and ice therapy. Physical therapy for these types of hernias focuses on pelvic muscles as well as abdominal muscles.
Minimally Invasive Surgical Repair
Surgical Treatment Options for a Hernia
Our surgeons will perform a thorough evaluation of each patient before developing the individualized plan that will be most effective. This may include recommendations to help the patient improve their overall health prior to having surgery to allow them the greatest chance for a successful repair. Non-surgical treatments can include rest, anti-inflammatory medications, and physical therapy to strengthen core muscles.
Patients with severe tears or unresolved symptoms may require surgery. Procedures include:
Open (with an incision) repairs
- Suture Repair - Some smaller hernia defects may be repaired with only a few stitches
- Mesh– The surgical area is reinforced with mesh that allows for greater tissue healing and strength. It results in a more lasting repair with a lower rate of recurrence. Mesh repair offers reinforcement but has pros and cons. Patients should be informed about the use of synthetic vs biologic mesh.
Minimally invasive
- Laparoscopic repairs - This type of minimally invasive repair often is performed through three to four small incisions (usually a half-inch or less).
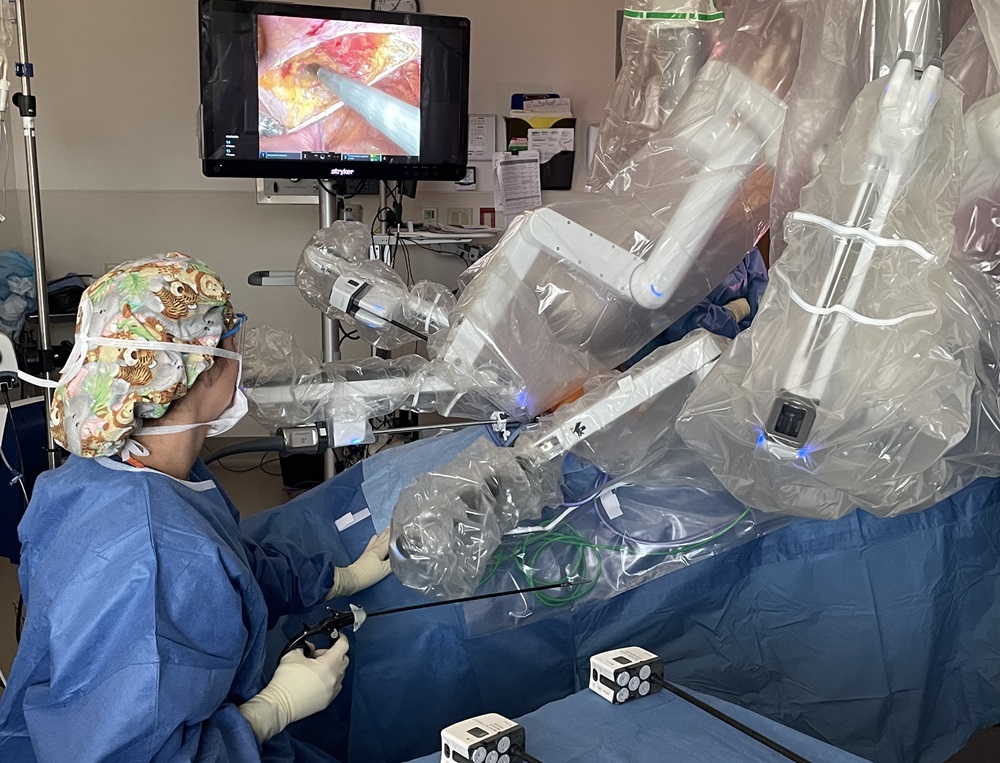
- Robotic repairs – Similar to laparoscopic, robotic repair uses advanced instruments controlled by the surgeon. This enables more types of complex hernias to be repaired with minimally invasive techniques.
Surgical Risks
There are common risks to any type of surgery and the associated use of anesthesia, such as bleeding, wound complications, development of blood clots, breathing difficulties and cardiac complications. The risk of these events is very low for most hernia surgeries. Other risks are more specific to each type of surgery:
- Groin hernias- trouble urinating right after surgery, long-term groin pain, hernia recurrence
- Ventral hernias– risks similar to the groin hernias, including recurrence, but also the risk of injury to the organs located inside your abdomen, fluid collections around the mesh, and other wound complications

Mesh
Almost all hernia’s larger than a very small size will benefit from mesh to decrease the recurrence rate. The size of hernia where mesh is a benefit is based on location. Tissues surrounding a hernia are uniformly weaker and will not be as strong as synthetic mesh reinforcement which is typically two to 10 times stronger than healthy body tissue.
Is mesh dangerous?
There are many types of mesh. Hernia meshes typically are made from multiple configurations of polypropylene plastic, polyester plastic, and Gore-Tex. The biggest risk of complication is related to location of mesh and the construction of the material. Mesh is not appropriate for all patients and the risks and benefits will be considered individually. All minimally invasive inguinal hernias require mesh, as do most minimally invasive ventral hernias. Meshes have been shown to decrease pain and shorten recovery time, in addition to decreasing the potential for hernia recurrence.