Changing Clinical Practice Through Training: High-Performance CPR-Resuscitation
Cardiac arrest can be a terrifying situation to encounter, even within the hospital. One of the greatest discoveries in the treatment of cardiac arrest was cardiopulmonary resuscitation (CPR). Though the concept of CPR as we know it dates back to 1960, research continues today to gain a better understanding of CPR and how it affects patient outcomes. No longer is it considered a “bridge” between first-responders and those trained to offer Advanced Cardiac Life Support (ACLS); rather CPR has become the central focus to improve chances of survival from cardiac arrest. The article below describes how CPR and cardiac arrest management have evolved to improve performance and save more lives.
The TriHealth Center for Simulation & Education offers many training courses in teamwork & communication (called non-technical skills), specialty topic courses, and high-risk/low volume training to name a few; mainly with the use of human patient simulators (HPS). In many of these courses, the “patient” simulators can and often do deteriorate into cardiac arrest. Course participants then deliver the same resuscitative measures in real time (to the simulators) including CPR, defibrillation, and pharmacological interventions through the same team dynamics as they would with real patients. It is important to note that the trainers we use and the methodologies that we teach are in line with the Emergency Cardiovascular Care guidelines from the American Heart Association (AHA); but these simulators go well beyond the traditional CPR manikin. The high-tech simulators are used in clinical training to measure CPR success, but to also teach teams how to handle stress-filled environments along with resource allotments and equipment that is seldom used. The simulators blink, breathe, talk and move respiratory gases in and out in real time. It is a very safe way to practice before reaching any patient.
The AHA concurred with published studies that without proper CPR training among teams, patient survival rates were likely to be significantly lower. With no formal training programs currently in place at TriHealth to improve performance of our teams during cardiac arrest, the TriHealth Center for Simulation and Education has taken the lead to improve survivability within our system.
To develop training techniques modeled after high-performing institutions, the TriHealth Center for Simulation and Education turned to the West Coast of the United States, specifically King County, Washington. Many national and international studies begin here where new concepts are put into place, first as a trial and then approval as a definitive treatment or standard of care. TraumaScope 2015 featured keynote speaker Mike Helbock, who is a faculty member of the Resuscitation Academy in King County. The primary mission of the Resuscitation Academy is to improve survival from cardiac arrest. Subsequently, by doing this, they have changed resuscitation strategies throughout the world. His presentation inspired us to dissect the profound differences between their method of high performance resuscitation and our attempt at cardiac arrest management.
The Resuscitation Academy successfully designed and implemented their system to become a nationwide model known as high performance CPR/resuscitation. Also referred to as “Pit Crew CPR,” coordination of the team within the resuscitation are choreographed much like one would see in auto racing where each pit crew member concentrates on one assigned task. Mr. Helbock was able to show how this pit crew philosophy has been carried over into medicine. By developing and implementing this program, King County has improved survival-to-discharge statistics in their area from 26% in 2002 to a staggering 62% in 2013.
High performance resuscitation is a way of utilizing the people and resources available to maximize survivability from cardiac arrest. It represents more than “do better chest compressions” or “buying time until the code team arrives”; high performance resuscitation is a cultural shift that begins with training, then execution, and finally review of performance standards.
Likewise, there are a few key concepts in this form of resuscitation. One key component is termed the compression fraction. This is the percentage of time that a patient receives chest compressions during a resuscitative effort. With continuous chest compression provided to a patient who is in cardiac arrest, perfusion to the heart and brain increases. Perfusion to these two vital organs is quantified by coronary perfusion pressure (CPP) and cardiocerebral resuscitation (CCR). Every pause for rhythm analysis, defibrillation, rescue breaths, and other interventions contributes to a decrease in compression fraction, and subsequent reduction in CPP and CCR; whereas purposeful control of interruptions to maximize compression fraction increase odds of survival (Chart 1).
Chart 1: Pathway 1 is desirable objective

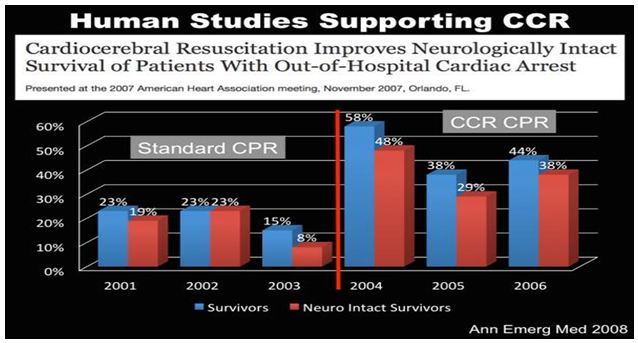
Clinical studies have proven that these variables, while working in tandem, must be maintained in order to achieve any chance of survival for the patient, especially for neurologically intact survival (Figure 1).
Figure 1:
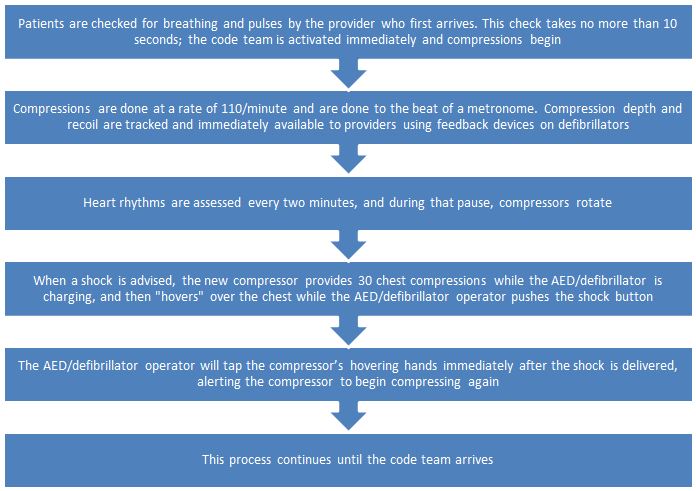
The techniques implemented in high performance resuscitation build upon skills that are learned in BLS and ACLS programs through the AHA. (Chart 2)
Chart 2:
When the code team arrives it is important for them to integrate with the team, rather than take over. This is when an effective report should be given and ACLS therapies should be considered. However, advanced skills should not take priority or be done in any way that sacrifices the integrity of the high performance resuscitation metrics mentioned above. By preventing interruptions for these skills (i.e. intubation, IV/IO access, etc.), we are increasing the compression fraction.
While all the above elements represent technical medicine and skills, other elements also play a major role in the resuscitation team’s performance. Teamwork, multidisciplinary collaboration, and effective communication are keys that not only improve the compression fraction, but provide an improved survival rate for patients experiencing cardiac arrest. Therefore a change in how many compressions we do, or how deep we push on the chest, or how frequently we deliver oxygen are not the “simple fixes” needed at TriHealth.
For the concept of high performance resuscitation to be implemented successfully at TriHealth, training and practice are essential. While annual Heartcode allows one person (at a time) to practice isolated parts of CPR, other forms of training must be supplemented to develop the high performance technique and choreography of a team in a clinical setting. Sophisticated human patient simulators and specially trained staff are also needed to facilitate training. The TriHealth Center for Simulation and Education offers just that through Code Readiness courses available to any department. Contact the Center at (513) 865-1415 or simulation_center@trihealth.com for more information or to schedule your staff.